Young People Admitted to Psychiatric Facilities Face Higher Risk of Self-Harm After Discharge, Researchers Say

Research has found that patients hospitalized for psychiatric treatment have higher risks of self-harm and suicide than psychiatric patients who were not hospitalized; even years after discharge, the previous inpatients were still at higher risk.

Psychiatric patients have an increased risk of suicide if they were forcibly hospitalized for treatment, a form of coercion the World Health Organization opposes as both ineffective and harmful to patients, who may feel dehumanized, disempowered and disrespected.
Other research also found that psychiatric hospitalization – and even psychiatric treatment without hospitalization – is linked to increased risk of suicide.
Using two years of data from the French national health records, the researchers investigated the risks of self-harm and death in more than 70,000 young people, aged 12 to 24 years, with psychiatric diagnoses who received treatment in a psychiatric hospital, as compared to control groups of young people with or without psychiatric diagnoses who were not treated in a psychiatric hospital.
During a 3-year follow-up, 57.6% of the hospitalized psychiatric patients were re-admitted to a psychiatric hospital an average of five times, starting an average of three months after their first hospitalization. That rate of hospitalization was 50% higher than the rate (38.2%) of hospitalization for the psychiatric patients who had not been initially hospitalized.
Among the young psychiatric patients initially hospitalized, 9.9% were re-hospitalized for self-harm, which includes attempted suicides. That rate of re-hospitalization was nearly 50% higher than the 6.8% rate of hospitalization for self-harm by those with psychiatric diagnoses who had not been initially hospitalized.
Among the initially hospitalized psychiatric patients, 0.8% died from any cause during the 3-year follow-up, with suicide accounting for almost half (42.8%) of the deaths. That death rate was twice the rate (0.4%) for the psychiatric patients who had not been initially hospitalized.
The researchers, publishing their study in Evidence-Based Mental Health, noted that the rates of self-harm and death among the young psychiatric patients who had been hospitalized initially were “significantly higher” than the rates not only for the youth with no psychiatric diagnoses, but also the patients with psychiatric diagnoses who were not initially hospitalized, suggesting that psychiatric hospitalization is a major factor in the significantly worse outcomes. [1]
With regard to the young people who had been treated in a psychiatric hospital, “we found that 1 in 10 individuals aged 12-24 years old will be hospitalized for a self-harming behaviour in the three years following discharge…and 1 in 100 will die, mostly from suicide but also from natural causes,” wrote lead author Fabrice Jollant, psychiatry professor at Jena University Hospital in Germany.
These findings are consistent with other research on psychiatric hospitalizations. A meta-analysis of 100 studies, published in JAMA Psychiatry in 2017, found that the suicide rate was approximately 100 times the typical global suicide rate during the first 3 months after discharge from a psychiatric facility. Patients admitted with suicidal thoughts or behaviors had rates nearly 200 times the global rate. Even many years after discharge, previous psychiatric inpatients had suicide rates that were approximately 30 times higher than typical global rates. [2]
A 2014 study published in Social Psychiatry and Psychiatric Epidemiology found that admission to a psychiatric facility in the preceding year was associated with a 44 times greater risk of suicide compared to those who did not receive any psychiatric treatment and that even individuals who received psychiatric treatment but were not admitted to a psychiatric facility were at a highly increased risk of suicide. [3]
Being forcibly committed to a psychiatric facility also increases the risk of suicide, according to still other research. A 2020 study, published in Suicide and Life-Threatening Behavior, found that people who perceived their admission to a psychiatric facility was coerced were more likely to attempt suicide after being released than those who did not. [4]
The World Health Organization (WHO) has taken a stand against forced mental health treatment, including involuntary commitment to a psychiatric facility, as both ineffective and harmful. In guidance issued in June 2021, it called on United Nations member nations to take action to end coercive mental health practices, which “are pervasive and are increasingly used in [mental health] services in countries around the world, despite the lack of evidence that they offer any benefits, and the significant evidence that they lead to physical and psychological harm and even death.” [5]
“People subjected to coercive practices report feelings of dehumanization, disempowerment, being disrespected and disengaged from decisions on issues affecting them,” according to the report. “Many experience it as a form of trauma or re-traumatization leading to a worsening of their condition and increased experiences of distress.”
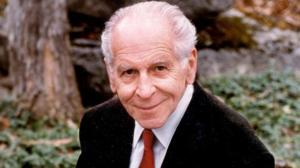
Co-founder of the Citizens Commission on Human Rights (CCHR), the late psychiatrist and humanitarian Thomas M. Szasz, a professor of psychiatry considered by many academics to be modern-day psychiatry’s most authoritative critic, wrote: “The most important deprivation of human and constitutional rights inflicted upon persons said to be mentally ill is involuntary mental hospitalization.” [6]
CCHR has been a global leader in the fight against the coercive and abusive use of involuntary commitments, seclusion and restraints, psychiatric drugs, and electroshock. In 1969, CCHR issued a Mental Health Declaration of Human Rights that laid out fundamental human rights in the field of mental health to ensure the right to one’s own mind, which includes the right to be free from forced mental health treatment. [7] Since then, CCHR has been instrumental in obtaining 228 laws against psychiatric abuses and violations of human rights worldwide.
The CCHR National Affairs Office in Washington, DC, has advocated for mental health rights and protections at the state and federal level. The CCHR traveling exhibit, which has toured 441 major cities worldwide and educated over 800,000 people on the history to the present day of abusive and racist psychiatric practices, has been displayed at the Congressional Black Caucus Foundation Annual Legislative Conference in Washington, DC, and at other locations.
[1] https://ebmh.bmj.com/content/25/4/177
[2] https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2629522
[3] https://pubmed.ncbi.nlm.nih.gov/24647741/
[4] https://pubmed.ncbi.nlm.nih.gov/31162700/
[5] https://www.who.int/publications/i/item/9789240025707
[6] https://www.cchrint.org/about-us/co-founder-dr-thomas-szasz/quotes-on-involuntary-commitment/
[7] https://www.cchr.org/about-us/mental-health-declaration-of-human-rights.html
Anne Goedeke
Citizens Commission on Human Rights, National Affairs Office
+1 202-349-9267
email us here
Visit us on social media:
Facebook
Dr. Thomas Szasz Tribute- Psychiatrist, Acclaimed Author & CCHR Co-Founder
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.