The Laboratory Science Behind Next-Gen Covid Vaccines

In early 2020, Formaspace responded to an emergency call from GM to build factory workstations for their new ventilator assembly plant.
Find out why the FDA approved next-generation Covid vaccines from Moderna and Pfizer targeting the Omicron variants BA.4 and BA.5.
In this Formaspace.com laboratory research article, we look at the science behind Moderna and Pfizer’s next-generation Covid mRNA vaccines, including some concern about the speed of the approval process.
Looking back at our first article on Covid from March 2020 – Laboratories Around the World are Collaborating on a Coronavirus Vaccine – it’s clear how much has changed. At that time, vaccine researchers were working against a relatively “fixed” viral target, the original SARS-CoV-2 virus (today known as the “wild-type” of Covid, or WT).
However, in the two years since we wrote our first lab science article on Covid, the world has experienced successive “waves” of new Covid variants (including Alpha, Beta, Gamma, Delta, Zeta, Mu, and Omicron) that “outcompeted” viruses in circulation to become the newest dominant variant.
Of these, Omicron and its sub-variants have become the most easily transmitted – especially the sub-variant BA.5, which appears to be capable of infecting individuals even when they are socially distancing outdoors.
Why Are First-Generation Moderna/Pfizer MRNA Covid Vaccines Less Effective Against Omicron Variants, Including BA.5?
Unfortunately, these Omicron variants are not only more transmissible, but they also can create “immune escape” infections that evade the first-generation mRNA vaccines.
Why is this?
First, a little recap on the mRNA vaccine mechanism.
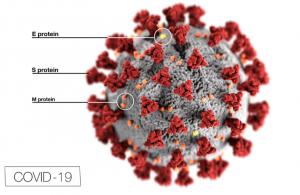
The first-generation mRNA vaccines from Pfizer and Moderna inject RNA molecules (encapsulated in a lipid jacket) into the body, where they enter cells and begin to rapidly replicate – creating copies that mimic the distinctive spike protein found on the surface of the original wild-type SARS-CoV-2 virus. These replicated RNA molecules generate an immune response, essentially teaching the immune system to be prepared to fight this new invader the next time it encounters it.
However, new Omicron sub-variants have mutated significantly from the original wild-type SARS-CoV-2 virus, especially in the spike region, rendering the original mRNA vaccines less effective in preventing infection.
A newly published paper in Science Immunology maps out the “antigenic cartography” of the different Covid variants, confirming that Omicron sub-variants BA.1 and BA.2 are significant antigenic outliers as compared to previous all variants – in other words, the obvious characteristics (such as the “spike” protein structure) have changed so much that the original first-generation mRNA vaccines are “training” the immune system to look for the wrong thing.
Another recent paper published in Nature sought to quantify the specific changes to the molecular surface of the different Omicron sub-variants. The researchers found that BA.1 variants had three mutations to the spike (L452Q, L452R, and F486V) that foiled antibodies from the mRNA vaccines or those generated naturally from previous pre-Omicron infections.
Frustratingly, researchers found the BA.4/BA.5 variants changed the game again. These variants have further mutations (S371F, D405N, and R408S) that not only evade pre-Omicron antibodies (whether naturally occurring or elucidated via vaccines) but ALSO evade antibodies generated from a naturally occurring BA.1 infection.
In other words, becoming infected with BA.1 does not appear to give people as much immune protection from a later BA.4/BA.5 infection as you might expect.
This could explain how some unfortunate individuals can experience multiple bouts of Covid – these might be caused by exposure to different variants over time. The situation is further complicated by the tendency of the human immune system to retain a high immune reaction to the very first Covid infection encountered, a phenomenon known as “original antigenic sin.”
Why Have So Many Covid Variants Arisen So Quickly? The Answer May Be Long-Covid Patients.
Why have so many Covid variants arisen so quickly?
One explanation is that this should be expected – viruses typically mutate over time to survive.
Read more...
Julia Solodovnikova
Formaspace
+1 800-251-1505
email us here
Visit us on social media:
Facebook
Twitter
LinkedIn
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.